Home training device for the deep spinal muscles
Table of contents
1 Back pain affects everyone
1.1 Back pain is an epidemic
1.2 Cause of back pain
2 A special muscle
2.1 The location of the multifidus
2.2 The function of the multifidus
2.3 Multifidus and back pain
3 Training device for the multifidus
3.1 MedX lumbar extension therapy device
3.2 Training the multifidus with a home training device
4 Bibliography
1 Back pain affects everyone
Out of necessity, I built a training device to effectively train certain back muscles. The background to why I did that is explained below.
The knowledge needed to understand my intentions behind it is a mix of scientific literature, anatomy and mechanics. Reading the text gives you also a good understanding of one of the main causes of back pain.
The journey to building the device began for me with back pain in the lumbar region. I would rate my physical health (mid-30s, 15 years of fitness training, never overweight, never smoked, little alcohol, insulin sensitive, etc.) as being in the 99th percentile of society. So why do I have back pain?
1.1 Back pain is an epidemic
It seems as if everyone knows someone who has back pain. A quick search in the literature explains the reasons. Back pain is considered one of the biggest health problems worldwide [1]. In the USA, it is estimated that the costs caused by lower back pain (LBP) amount to at least $50 billion[2] per year. In Switzerland, the costs caused by LBP are estimated to be at least 1.6%[3] of GDP each year. And the trends point to the situation getting worse.
Why can't we get back pain under control?
1.2 Cause of back pain
Apart from some more obvious causes, such as a previous accident, the cause of LBP is difficult to determine in most cases. In general, studies[4] [5] [6] [7] show that there is only a weak or no correlation between LBP and age/body weight/gender/smoking/etc. The complexity of determining the cause is particularly evident when looking at the “classic” herniated disc. It is generally known that a herniated disc causes tears in the annulus fibrosus, which in turn causes disc tissue to press on nerves and thus cause pain (Fig. 1). What is strange, however, is that over 20% of people with a herniated disc do not experience any pain[8].
This all sounds frustrating up to this point. Does science not offer a solution?

Figure 1: Herniated disc
2 A special muscle
In the next few sections, I would like to give the reader the basic knowledge needed to clearly identify the problem of back pain. I will concentrate on the essentials in order to keep the format of this text as compact as possible.
2.1 The location of the multifidus
Let's imagine we are standing behind a person and looking at their back. Under the skin there is a layer of muscle called the "superficial muscle group". Muscles that lie under this layer are called the "intermediate muscle group". Another layer "deeper" is the "deep muscle group". Having reached the "deepest" level, we can now see our target. The (lumbar) spine and some smaller muscle groups that are directly connected to the spine. There we find the so-called "lumbar extensor muscles". The so-called multifidus muscles are crucial for us. These small muscles run along the spine and connect up to 5 vertebrae with each other (Fig. 3).
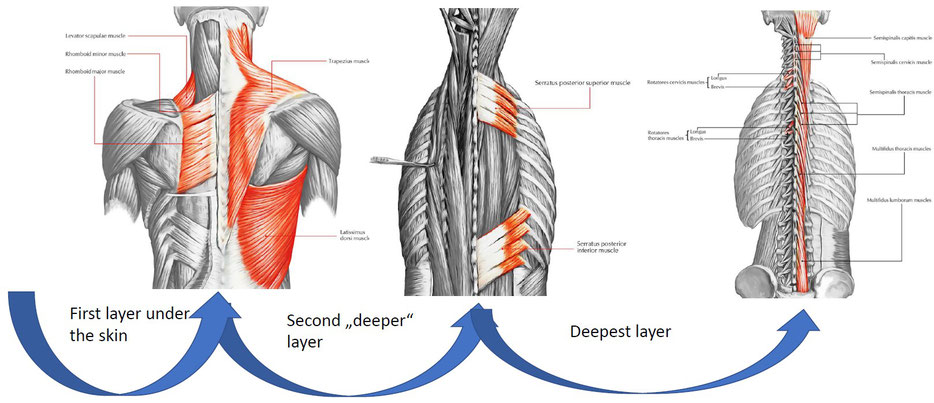
Figure 2: Different layers of the back muscles

Figure 3: Multifidus muscle
2.2 The function of the multifidus
Muscles do work by contracting. This means they create a movement in one direction via a joint. A short physics problem will enable us to better estimate the forces that muscles normally have to exert in order to be able to carry out our everyday tasks. Let's assume someone is lifting a 4 kg object in their hand (Fig. 4). Now we want to calculate how much force the biceps has to exert.


Figure 4: Lever law on the human body
The arm and the weight are pulled down by the earth with 64 N. The ratio of 470 N to 64 N is 7.3. Due to the poor leverage ratio, the biceps must therefore exert over 7 times the force to be able to hold the hand in the horizontal position. The multifidus, on the other hand, works more efficiently, similar to a pair of pliers (Fig. 5), and can effectively exert about twice the force used (this will be important later to better interpret measurement results).

Figure 5: Lever law at the multifidus muscle
By measuring [9] [10] the electrical currents in the muscles (electromyography), we know that the multifidus is "active" when we:
- Stand still
- Bend forward
- Pick things up
- Walking
And is "inactive" when we
- Spin on our own axis
- Bend backward without counterweight
- Ly down
Active does not mean that the multifidus does the work of "lifting". What the muscle does is called proprioception [11]. Simply put, this means that the muscles tell the brain where the vertebrae are in space. The brain "calculates" which positional corrections are necessary based on the current situation so that the vertebrae are ideally positioned relative to one another. The muscles then carry out these corrections (Fig. 6).

Figure 6: Proprioception principle at the multifidus muscle
There are more features of the multifidus, but by this point it should be clear that the muscle is quite different from more familiar muscles. It is an important part of spinal movement and is close to the center of back pain.
2.3 Multifidus and back pain
I mentioned at the beginning that it is difficult to find a correlation between back pain (LBP) and factors such as obesity, age, etc. However, a completely different picture emerges when we focus on studies that look at the multifidus in combination with LBP. Then it quickly becomes clear that a diseased multifidus is de facto always associated with LBP. Before I list some of the many studies on this, I would like to briefly explain what the two main causes of a diseased muscle are.
Firstly, muscle atrophy. This means a weak or underdeveloped muscle. The cause of this is usually a muscle that is not used enough.
The second main cause is myosteatosis. To understand this term, you have to know that the body has a regular fat storage. And these are the so-called adipocytes or fat cells. Mostly due to an unhealthy lifestyle, many people force their bodies to store fat in areas that are not intended for it (ectopic fat deposits such as visceral fat). This is fat on the organs and fat on the muscles, called myosteatosis. In summary, it can be said that fat in the fat cells is OK, but fat on the organs/muscles is very bad.
Here are some studies on the topic of multifidus muscles and back pain:
- Study[11] examined multifidus muscle size in 80 people (15-18 years old).
Result: People suffering from LBP had significantly smaller (weaker) multifidus muscles.
- Study[12] examined multifidus muscles in 78 people (17-72 years old).
Result: People suffering from LBP had atrophy and myosteatosis of the multifidus. In addition, many of the people also had leg pain.
- Study[13] examined multifidus muscles in 90 people.
Result: People suffering from LBP had atrophy of the multifidus. (especially in the lowest vertebrae L4 and L5)
- Study[14] examined multifidus muscles in 132 people with a herniated disc.
Result: Almost all people with a herniated disc had multifidus atrophy.
- Study[15] examined multifidus muscles in 23 professional football players with LBP.
Result: LBP correlated strongly with multifidus muscle size.
There are many more studies that all show the same thing:
A healthy, strong multifidus muscle reduces greatly the likelihood of back pain.
The best way to achieve this is with muscle training.
3 Training device for the multifidus
For the lower back area, fitness equipment such as that shown in Figure 7 is usually available.

Figure 7: Typical training equipment for training the lower back
With such standard equipment, the multifidus muscle is trained inefficiently at best and usually not at all.
A company in the USA found out why this is the case in the late 1980s.
3.1 MedX lumbar extension therapy device
In 1986, Arthur Jones founded the company MedX in the USA. In collaboration with the University of Florida, after years of development and an investment of around 100 million dollars, they released medical training and measuring devices. The MedX LE Lumbar Extension device is crucial for back pain. The complex development of the device is described in the book "The Lumbar Spine, The Cervical Spine And the Knee; Testing and Rehabilitation". After countless series of tests with many measurements on computer-aided device prototypes, they discovered something important:
Effective isolated training of the lumbar extensor muscles (multifidus) is only possible if the rotation of the pelvis is completely prevented. Otherwise, the muscles of the hips and thighs (gluteus and hamstrings) will do most of the work.
In Figure 8, the middle drawing shows schematically how a person must be clamped in so that in fact only the muscles of the lumbar spine do most of the work for the counterweight. This also limits the maximum possible back movement from approx. 110° to approx. 72°.

Figure 8: MedX lumbar extrension schematics
The MedX LE device is shown in Figure 9.

Figure 9: Original MedX lumbar extension
We now know that, in theory, effective training of the multifidus muscles should lead to an improvement in back pain, and we know that these can be effectively trained with the MedX LE. So there must obviously be appropriate studies that show that training with the MedX LE device helps with back pain.
- Study[16] with 627 people who had back pain (and some leg pain) examined the effects of training with the MedX LE device.
Result: The vast majority of people who trained on the MedX LE experienced a massive improvement in back pain (and some leg pain).
- Study[17] examined the effectiveness of training on the MedX LE with FullROM and LimROM on 24 people with LBP.
Result: In both cases, the training led to massive pain relief and some improvement in ROM (greater freedom of movement).
- Study[18] examined the effects of MedX training after surgery on 14 patients who had surgery for a herniated disc.
Result: The MedX group experienced significant pain relief (compared to the control group without training).
- Studies[19] [20] examined the effectiveness of standard training methods such as the Roman Chair, lower back devices, etc. (Fig. 7) for the lumbar extensor muscles in comparison to the MedX LE.
Result: The standard methods do not allow for effective training of the lumbar extensor muscles in comparison to the MedX LE.
There are countless other studies, but they all come to the same conclusion:
Back training with immobilization of the body below the pelvis leads to a huge improvement in back pain.
It turned out that a therapist about 100 km away from me had such a device. So I went there to have my back muscles measured. The measurement result is shown in Figure 10.

Figure 10: Measurements with a MedX LE
A very "weak" result, which would explain my back pain. So it was clear that I had to do something here. Every time I wanted to train on the "original device" I would have to drive 200 km and pay 50 euros. So I considered buying the home version of the machine. After several days of Google research, I realized that there is no such device for the multifidus muscles.
So I had to build one myself.
3.2 Training the multifidus with a home training device
After a few months of tinkering, I thought I had built a usable prototype with which I could train my multifidus muscles. So I trained with it once a week for 12 weeks and then went back to the MedX LE to take measurements. The result is the orange line in Figure 11.

Figure 11: Measurements with a MedX LE after training with the prototype
An obviously enormous increase in strength. And my back pain has also gone down. But how should we evaluate the enormous increase of over 100% after such a short time? Thanks to the understanding gained in Chapter 2.2, we know that the multifidus muscle uses the lever law much more efficiently than most muscles. That is the main reason for this enormous increase in such a short time.
Before I describe my device in more detail, I would like to briefly mention my original train of thought:
What I don't need to train the multifidus muscle (compared to MedX LE) includes:
- No precise measurement of strength
- No counterweights to counteract the body weight
- No computer-aided measurement
What I need:
- Immobilization from the pelvis downwards using a tensioning device
- Pivoting cushion on the pelvis (explanation below)
- Training weight
The tensioning device must in principle act in at least three places (Fig. 12, points A, B, C). Tension is applied in one place and this force must be counteracted in two places.

Figure 12: Working principle for a home training device
The pivoting cushion (point C) is necessary to determine whether the tension is large enough. If the cushion rotates during movement, the tension is too small and the body directs too much force towards the leg muscles. If only the lumbar extensor muscles are working, the tension is large enough and the cushion should not rotate in this case.
Under prototype one can find out more about the current version.
4 Bibliography
[1] GBD 2015 Disease and Injury Incidence and Prevalence Collaborators, “Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015,” Lancet Lond. Engl., vol. 388, no. 10053, pp. 1545–1602, Oct. 2016, doi: 10.1016/S0140-6736(16)31678-6.
[2] J. W. Frymoyer and W. L. Cats-Baril, “An overview of the incidences and costs of low back pain,” Orthop. Clin. North Am., vol. 22, no. 2, pp. 263–271, Apr. 1991.
[3] S. Wieser et al., “Cost of low back pain in Switzerland in 2005,” Eur. J. Health Econ. HEPAC Health Econ. Prev. Care, vol. 12, no. 5, pp. 455–467, Oct. 2011, doi: 10.1007/s10198-010-0258-y.
[4] P. Kjaer, N. Wedderkopp, L. Korsholm, and C. Leboeuf-Yde, “Prevalence and tracking of back pain from childhood to adolescence,” BMC Musculoskelet. Disord., vol. 12, p. 98, May 2011, doi: 10.1186/1471-2474-12-98.
[5] C. E. Dionne, K. M. Dunn, and P. R. Croft, “Does back pain prevalence really decrease with increasing age? A systematic review,” Age Ageing, vol. 35, no. 3, pp. 229–234, May 2006, doi: 10.1093/ageing/afj055.
[6] R. Shiri, J. Karppinen, P. Leino-Arjas, S. Solovieva, and E. Viikari-Juntura, “The association between smoking and low back pain: a meta-analysis,” Am. J. Med., vol. 123, no. 1, p. 87.e7–35, Jan. 2010, doi: 10.1016/j.amjmed.2009.05.028.
[7] T.-T. Zhang, Z. Liu, Y.-L. Liu, J.-J. Zhao, D.-W. Liu, and Q.-B. Tian, “Obesity as a Risk Factor for Low Back Pain: A Meta-Analysis,” Clin. Spine Surg., vol. 31, no. 1, pp. 22–27, Feb. 2018, doi: 10.1097/BSD.0000000000000468.
[8] S. D. Boden, D. O. Davis, T. S. Dina, N. J. Patronas, and S. W. Wiesel, “Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation,” J. Bone Joint Surg. Am., vol. 72, no. 3, pp. 403–408, Mar. 1990.
[9] J. P. Arokoski et al., “Back and hip extensor muscle function during therapeutic exercises,” Arch. Phys. Med. Rehabil., vol. 80, no. 7, pp. 842–850, Jul. 1999, doi: 10.1016/s0003-9993(99)90237-x.
[10] F. P. Valencia and R. R. Munro, “An electromyographic study of the lumbar multifidus in man,” Electromyogr. Clin. Neurophysiol., vol. 25, no. 4, pp. 205–221, Jun. 1985.
[11] N. Rahmani, A. Kiani, M. A. Mohseni-Bandpei, and I. Abdollahi, “Multifidus muscle size in adolescents with and without back pain using ultrasonography,” J. Bodyw. Mov. Ther., vol. 22, no. 1, pp. 147–151, Jan. 2018, doi: 10.1016/j.jbmt.2017.05.016.
[12] D. F. Kader, D. Wardlaw, and F. W. Smith, “Correlation between the MRI changes in the lumbar multifidus muscles and leg pain,” Clin. Radiol., vol. 55, no. 2, pp. 145–149, Feb. 2000, doi: 10.1053/crad.1999.0340.
[13] J. Hides, C. Gilmore, W. Stanton, and E. Bohlscheid, “Multifidus size and symmetry among chronic LBP and healthy asymptomatic subjects,” Man. Ther., vol. 13, no. 1, pp. 43–49, Feb. 2008, doi: 10.1016/j.math.2006.07.017.
[14] C. Liu et al., “Is there a correlation between upper lumbar disc herniation and multifidus muscle degeneration? A retrospective study of MRI morphology,” BMC Musculoskelet. Disord., vol. 22, no. 1, p. 92, Jan. 2021, doi: 10.1186/s12891-021-03970-x.
[15] J. A. Hides, T. Oostenbroek, M. M. Franettovich Smith, and M. D. Mendis, “The effect of low back pain on trunk muscle size/function and hip strength in elite football (soccer) players,” J. Sports Sci., vol. 34, no. 24, pp. 2303–2311, Dec. 2016, doi: 10.1080/02640414.2016.1221526.
[16] B. W. Nelson, E. O’Reilly, M. Miller, M. Hogan, J. A. Wegner, and C. Kelly, “The clinical effects of intensive, specific exercise on chronic low back pain: a controlled study of 895 consecutive patients with 1-year follow up,” Orthopedics, vol. 18, no. 10, pp. 971–981, Oct. 1995, doi: 10.3928/0147-7447-19951001-05.
[17] J. Steele, S. Bruce-Low, D. Smith, D. Jessop, and N. Osborne, “A randomized controlled trial of limited range of motion lumbar extension exercise in chronic low back pain,” Spine, vol. 38, no. 15, pp. 1245–1252, Jul. 2013, doi: 10.1097/BRS.0b013e318291b526.
[18] S. Ju, G. Park, and E. Kim, “Effects of an Exercise Treatment Program on Lumbar Extensor Muscle Strength and Pain of Rehabilitation Patients Recovering from Lumbar Disc Herniation Surgery,” J. Phys. Ther. Sci., vol. 24, no. 6, pp. 515–518, 2012, doi: 10.1589/jpts.24.515.
[19] J. L. Verna, J. M. Mayer, V. Mooney, E. A. Pierra, V. L. Robertson, and J. E. Graves, “Back extension endurance and strength: the effect of variable-angle roman chair exercise training,” Spine, vol. 27, no. 16, pp. 1772–1777, Aug. 2002, doi: 10.1097/00007632-200208150-00016.
[20] J. E. Graves et al., “Pelvic stabilization during resistance training: its effect on the development of lumbar extension strength,” Arch. Phys. Med. Rehabil., vol. 75, no. 2, pp. 210–215, Feb. 1994.
